Long covid: probably worth avoiding—some considerations
post by KatjaGrace · 2022-01-16T11:46:52.087Z · LW · GW · 88 commentsContents
A. Really bad anecdotes aren’t hard to find. B. Bad anecdotes are common enough to show up in my vicinity. C. Rates of ambiguously-maybe-quite-bad symptoms seem very high, even for people who only had mild covid D. It looks like a lot of people can no longer do their jobs E. Other people’s previous back of the envelope calculations on this are not reassuring. F. Having ‘survived’ covid looks associated with a 60% increased risk of death (after surviving covid) during the following six months G. Overall deaths from everything have been very unusually high at points in 2021, even in 15-64 age group H. Sounds like these things involve various damage throughout body, and my guess is that that ends up being regrettable in ways not captured in ‘hours lost to fatigue this year’ I. It’s easy to just think about these worst case outcomes, but there are a lot of more probable non-worst case outcomes that would still be a non-negligible bummer. J. Future unknowns K. Long covid probably isn’t psychosomatic L. The general discussion of what is going on with people’s brains sounds terrible M. It sounds like covid maybe persists in your body for ages? N. Later rounds of covid are probably bad too O. It’s not 100% that you will get it. P. The likelihood of you getting it probably does depend on how bad it is Q. Getting covid later is probably better than earlier. R. Huge VOI in following behind the crowd, at a safe distance None 89 comments
I hear friends reasoning, “I’ll get covid eventually and long covid probably isn’t that bad; therefore it’s not worth much to avoid it now”. Here are some things informing my sense that that’s an error:
A. Really bad anecdotes aren’t hard to find.
I asked for people’s long-covid experiences on Twitter and got more than a hundred comments mostly full of truly awful stories, almost entirely from people I don’t know at all, presumably somehow brought via the active Long Covid community.
This is a bit hard to interpret as a datum, due to the intense selection effects involved, but my main inferences are:
- The bad tail gets very bad.
- This bad tail is less like a quantitative reduction in labor, and more like psychological torment, being very sleep deprived or brain damaged while dealing with a host of legitimately scary health problems (see below) than I had been picturing.
- The very bad part of the bad tail is not tiny. Like, if I requested lightning strike experiences, I don’t think I would get this kind of response.
See this for more heavily selected but still scary anecdotes about what bad cases can look like.
B. Bad anecdotes are common enough to show up in my vicinity.
Among this cascade of terrible stories is a response from one of the handful of people from my extended network who I already knew had had covid, Oxford machine learning professor Michael Osborne. I take this as strong evidence that that level of bad experience isn’t vanishingly rare, though he has been well for the last few months, so this is only direct evidence of this kind of thing happening for about two years.
Excerpts from his account:
My own low-points: early on, I collapsed, shaking, and was taken to A&E in an ambulance. A year later, I did not have the energy to leave the house. Formerly, I was a marathon runner, but I brought on a bad relapse with a 700m walk. Many people have it much, much, worse. 2/
— Michael A Osborne (@maosbot) October 19, 2021
Brain fog is a bit like being extremely sleep-deprived—remember, sleep deprivation is literally a technique of torture—but you can't sleep off brain fog. It feels like being lost in a fog, sensing dark shapes shifting around you, losing yourself. 6/
— Michael A Osborne (@maosbot) October 19, 2021
"Fatigue" similarly does no justice to the experience. Fatigue means there is less of you. You are less. You can't, just can't, get out of bed. This is not psychological (although fatigue may cause depression!). Your body, physically, does not have the energy. 7/
— Michael A Osborne (@maosbot) October 19, 2021
(Another distant relative in my generation just told me that they have long covid, but I take that as much less evidence, since I only know about them having covid at all because they saw this long covid discussion.)
C. Rates of ambiguously-maybe-quite-bad symptoms seem very high, even for people who only had mild covid
This norwegian study, n = 70k, has, for mild cases (in a sample mixing people who had covid 1-6 months prior with people who had it 11-12 months prior):
- 10.2% with fatigue (6.4% higher than control in the 11-12 months case),
- 7.1% with poor memory (3.5% higher than previous control),
- 9.2% with brain fog (5.3% higher than previous control).
- 6.9% with shortness of breath (5.6% higher than previous control)
These numbers are for unvaccinated people; I’d maybe reduce them by a factor of two for being vaccinated, deferring to Matt Bell, who reasons, “A very recent report from the UK claims that full vaccination cuts the risk of lingering symptoms 28+ days after catching COVID by roughly half”.
This meta-analysis of 81 studies finds:
-
“Approximately 1 in 3 individuals experienced fatigue 12 or more weeks following COVID-19 diagnosis.”
-
“Approximately 1 in 5 individuals exhibited cognitive impairment 12 or more weeks following COVID-19 diagnosis.”
(Though I am told that lot of the studies involved might have been small-n, hospitalized, no control, so I’m not sure how they dealt with that.)
This survey suggests that among people with long covid (I think drawn from a support group), some especially undesirable symptoms are very: “88.0% of the total respondents (3310) experienced either cognitive dysfunction or memory loss (Figure 8).”
All of these symptoms come in degrees between slightly annoying and life-wrecking, making all of this hard to interpret. Maybe we can look at something more objective, like ‘can the person still do their job?’
D. It looks like a lot of people can no longer do their jobs
- Katie Bach of Brookings argued a few days ago that an estimate of 1.1 million people out of work because of long covid is reasonable, out of 103 million working age Americans she estimated had had covid, i.e. a roughly 1% chance of being entirely out of work:
- Washington post: “Hard data is not available and estimates vary widely, but based on published studies and their own experience treating patients, several medical specialists said 750,000 to 1.3 million patients likely remain so sick for extended periods that they can’t return to the workforce full time.”
- This meta-analysis of 81 studies I mentioned earlier also looked at work: “29.0% and 47.4% of those who were employed premorbidly were not able to return to work”; “5% to 90% were unable to reach their pre-COVID employment level” (p. 128) (As noted earlier, a lot of the studies in the meta-analysis seem to be small n, involving hospitalized people, without controls, and I don’t know what they did about this. Also, it’s possible I’m misunderstanding what group the meta-analysis is about, given how crazy high the numbers are).
Some harder to interpret data about long covid sufferers in particular (where I’m not sure how many people count as that) still suggests pretty major issues:
Matt bell says that this UK data-set has ~18% of non-hospitalized long covid sufferers with “activities limited a lot.”
And looking at a survey I mentioned earlier again, people with long covid (and probably under selection to be relatively bad cases) report large losses of ability to work, and in other specific capabilities:
- “The greatest area of impact reported was on work, with 86.2% (95% confidence interval 84.4 to 88.0%) of working respondents feeling mildly to severely unable to work - 29.1% (26.7% to 31.6%) severely…. Other areas of impact included making serious decisions 85.3% (80.7% to 89.8%), communicating thoughts and needs 74.8% (72.5% to 77.1%), having conversations with others 68.3% (65.8% to 70.8%), maintaining medication schedules 62.5% (59.8% to 65.1%), following simple instructions 54.4% (51.6% to 57.2%), and driving 53.2% (50.5% to 56.0%).” (p. 16)
- “Of unrecovered respondents who worked before becoming ill, only 27.3% (95% confidence interval 25.3% to 29.4%) were working as many hours as they were prior to becoming ill at the time of survey, compared to 49.3% (40.8% to 57.9%) of recovered respondents (see Figure 11d). Nearly half 45.6% (43.2% to 48.0%) of unrecovered respondents were working reduced hours at the time of the survey, and 23.3% (21.3% to 25.4%) were not working at the time of the survey as a direct result of their illness. This included being on sick leave, disability leave, being fired, quitting, and being unable to find a job that would accommodate them. The remaining respondents retired, were volunteers, or did not provide enough information to determine their working status. Overall, 45.2% (42.9% to 47.2%) of respondents reported requiring a reduced work schedule compared to pre-illness. 22.3% (20.5% to 24.3%) were not working at the time of survey due to their health conditions.” p. 27.
E. Other people’s previous back of the envelope calculations on this are not reassuring.
“If you’re a 35 year old woman, and your risk of ending up with lifelong long COVID from catching COVID is 2.8%, then catching COVID would be the same, statistically speaking, as losing (50 years * 0.18 * 0.028 * 365 days/year) = ~90 days of your life.”
“Your chance of really bad debilitating lifelong Long COVID, conditional on getting COVID, is probably somewhere between a few tenths of a percent, and a few percent.”
F. Having ‘survived’ covid looks associated with a 60% increased risk of death (after surviving covid) during the following six months
According to a massive controlled study published in Nature (more readable summary here). It also looks like they are saying that this is for non-hospitalized covid patients, though the paper is confusing to me.
I’m not sure whether to model this as some longer-than-a-few-weeks period of danger that is still done within the year (maybe 400 micromorts if done by six months), versus semi-permanently worse health (which would maybe be like aging about 8 years).
This is bad because death, but I’m maybe more alarmed by it because it supports the ‘post-covid illness is some fairly extreme body fuckage of which the fact that some people can’t think straight is merely a tip-of-the-iceberg symptom’ hypothesis over the ‘most of the story is that you lose some work time this year’ hypothesis. Both because death really suggests something wrong, and because they catalogue a lot of things wrong—from the WebMD summary: “The patients had a high rate of stroke and other nervous system ailments; mental health problems such as depression; the onset of diabetes; heart disease and other coronary problems; diarrhea and digestive disorders; kidney disease; blood clots; joint pain; hair loss; and general fatigue.”
It’s also a bad sign about what a bad time you might have during that year. I don’t think these people go gently - it seems like a repeating theme of these long covid stories is that their victims have a lot of health scares and medical investigation, and this mortality data suggests to me that they are genuinely at risk of their lives, which I think would make the experience much worse, for me at least.
G. Overall deaths from everything have been very unusually high at points in 2021, even in 15-64 age group
(The Center Square) – The head of Indianapolis-based insurance company OneAmerica said the death rate is up a stunning 40% from pre-pandemic levels among working-age people.
“We are seeing, right now, the highest death rates we have seen in the history of this business – not just at OneAmerica,” the company’s CEO Scott Davison said during an online news conference this week. “The data is consistent across every player in that business.”
OneAmerica is a $100 billion insurance company that has had its headquarters in Indianapolis since 1877. The company has approximately 2,400 employees and sells life insurance, including group life insurance to employers nationwide.
Davison said the increase in deaths represents “huge, huge numbers,” and that’s it’s not elderly people who are dying, but “primarily working-age people 18 to 64” who are the employees of companies that have group life insurance plans through OneAmerica.
“And what we saw just in third quarter, we’re seeing it continue into fourth quarter, is that death rates are up 40% over what they were pre-pandemic,” he said.
“Just to give you an idea of how bad that is, a three-sigma or a one-in-200-year catastrophe would be 10% increase over pre-pandemic,” he said. “So 40% is just unheard of.”
H. Sounds like these things involve various damage throughout body, and my guess is that that ends up being regrettable in ways not captured in ‘hours lost to fatigue this year’
See Nature study in F. I also feel like I’ve seen this a lot, but don’t have that many examples immediately on hand. Here’s one other example, not ideal because note that these are hospitalized younger people:
For people younger than 65 who were hospitalized with COVID-19, the risk of death in the 12 months after the infection was 233% higher than it was for people who did not have the disease, results published in the journal Frontiers in Medicine have shown.
Nearly 80% of all deaths of people in the study who had recovered from COVID-19 in the past 12 months were not due to cardiovascular or respiratory causes, suggesting that the impact of the virus is significant and wide-ranging, even after the initial infection has been fought off.
My guess is that all the symptoms are a spectrum, and if the worst looks like an unbelievable amount of cognitive impairment and a pot pourri of organ dysfunctions, or death post-infection, then probably everyone gets a handful of cognitive impairment and organ dysfunction.
I. It’s easy to just think about these worst case outcomes, but there are a lot of more probable non-worst case outcomes that would still be a non-negligible bummer.
I see people mostly estimating the worst cases, but my guess is that the more probable non-worst case outcomes (e.g. lesser fatigues and brain fogs, kidney damage, arrhythmias etc), are not nothing.
J. Future unknowns
Across all diseases, how much of their disutility is obvious in the first two years? Saliently right now: we’ve had Epstein-Barr for ages and only now noticed that it apparently has a ~1/300 chance of causing MS, usually showing up between 20 and 40, long after the virus, and wreaking brutal destruction. I’m not sure whether we would realize how bad HIV was if it had appeared two years ago and lots of people had it, but nobody had had it for more than two years yet.
K. Long covid probably isn’t psychosomatic
A French study found that long covid is barely associated with having had covid according to an antibody test, yet associated with believing one has had covid (which itself is unrelated to the antibody test results).
At first I (and I think others) thought that if this wasn’t some error, then long covid was likely psychosomatic and not caused by physically having covid. But on further thought, that’s totally wrong: this pattern could be caused by beliefs causing illness, but it could also be caused by illness causing beliefs, which obviously happens all the time. That is, people’s guesses about whether they had covid are heavily influenced by their symptoms.
Imagine a population of a thousand people. A hundred of them get covid this year, and ten get long covid caused by the virus. Fifty and five of those respectively notice that they have covid at the time. Also a hundred people get other illnesses that look like long covid (other viral infections, other mental health problems, other random things). Everyone knows that a lot of people are getting covid and don’t know they have covid. The hundred people who got some other illness that looks like long covid infer that they are plausibly in the asymptomatic covid group, since they seem to have long covid. Especially the ones who got some viral illness, so were actually a bit sick at around the time they developed their chronic illness. So we end up with people who think they have long covid having less covid than the general population, even though long covid caused by the covid virus is genuinely afflicting 10% of the covid infected. Note that everyone here might have non-psychosomatic illnesses.
It seems to me that we have other data that basically rules out the possibility that long covid is imaginary (e.g. see Nature study above on laboratory abnormalities and raised death rate). Though psychosomatic illness is weird - my understanding is that it could in principle still be psychosomatic, while yielding measurable physical laboratory abnormalities, though intuitively I’d be fairly surprised to learn that the same new psychosomatic syndrome had gripped millions in the wake of a particular belief they had, and raised their risk of death by half. Maybe I’m missing something here.
L. The general discussion of what is going on with people’s brains sounds terrible
The list of different plausible routes to brain damage occurring according to Nature—some brain cells getting broken, some blood restrictions causing little strokes, some immune system attacking your own brain type issues—is one I want very little to do with. For instance:
“…The researchers observed that, in slices of hamster brain, SARS-CoV-2 blocks the functioning of receptors on pericytes, causing capillaries in the tissue to constrict. “It turns out this is a big effect,” says Attwell.
It’s a “really cool” study, says Spudich. “It could be something that is determining some of the permanent injury we see — some of these small-vessel strokes.”“
Another sample of current discussion of the brain damage situation that I really don’t want to be a part of, this time from NPR:
Frontera led a study that found that more than 13% of hospitalized COVID-19 patients had developed a new neurological disorder soon after being infected. A follow-up study found that six months later, about half of the patients in that group who survived were still experiencing cognitive problems.
The current catalog of COVID-related threats to the brain includes bleeding, blood clots, inflammation, oxygen deprivation and disruption of the protective blood-brain barrier. And there’s new evidence in monkeys that the virus may also directly infect and kill certain brain cells…
“Frontera was part of a team that studied levels of toxic substances associated with Alzheimer’s and other brain diseases in older COVID-19 patients who were hospitalized.
“The levels were really high, higher than what we see in patients that have Alzheimer’s disease,” Frontera says, “indicating a very severe level of brain injury that’s happening at that time.”…
Even COVID-19 patients who experience severe neurological problems tend to improve over time, Frontera says, citing unpublished research that measured mental function six and 12 months after a hospital stay.
“Patients did have improvement in their cognitive scores, which is really encouraging,” she says.
But half of the patients in one study still weren’t back to normal after a year….”
M. It sounds like covid maybe persists in your body for ages?
Seems like the virus lives throughout your organs long after recovery, based on autopsies, including of mild/asymptomatic covid sufferers (summary, paper):
“The study found that the virus had replicated across multiple organ systems even among patients with asymptomatic to mild COVID-19.
The virus was detected in all 44 cases and across 79 of 85 anatomical locations and body fluids sampled”
“We performed 72 complete autopsies on 44 patients with COVID-19 to map and quantify SARS-CoV-2 73 distribution, replication, and cell-type specificity across the human body, including brain, 74 from acute infection through over seven months following symptom onset. We show that 75 SARS-CoV-2 is widely distributed, even among patients who died with asymptomatic to 76 mild COVID-19, and that virus replication is present in multiple pulmonary and 77 extrapulmonary tissues early in infection. Further, we detected persistent SARS-CoV-2 78 RNA in multiple anatomic sites, including regions throughout the brain, for up to 230 days 79 following symptom onset.”
This seems like a bad sign for future problems.
Ok, that was ‘covid is bad, primarily due to long covid’. But aren’t we all going to get it anyway?
N. Later rounds of covid are probably bad too
This assumes that later covids are basically free, once you’ve done it once, in a way that isn’t true for e.g. crashing your car. My guess is that later bouts are less bad on average, but far from free.
In my survey, of three people with lasting problems who got covid at least twice, one got the problems with the first, one the second, and one said both contributed (though for the last person, the second was around a month ago). Not a great sample size, but seems like strong evidence that second-round long-covid isn’t unheard of.
O. It’s not 100% that you will get it.
I’d guess there’s a decent chance you’ll be able avoid it, via reasonable-to-pay costs. For instance, maybe omicron basically brings herd immunity. Maybe rapid tests get more reliable, easy, and cheap. Maybe long covid becomes a bigger concern, and people worry enough to get R0 generally below 1. Or other technologies improve: Fend really does cut covid exhalations massively and is taken up widely, or something like Novid finds a way to be taken up. (Or your path takes you to being a hermit or living in China, or we spend next year hiding in bunkers from cyborg bees, and you are glad you didn’t pay all that covid risk up front for parties that aren’t happening.)
(If we were doing exactly what we are doing so far, but with air purifiers in most buildings, would R0 would have been ¼ instead of ~1, and would it have died out? Is the problem that we are psychologically incapable of maintaining slightly more caution than needed to keep infections steady?)
Are things so predictable?
P. The likelihood of you getting it probably does depend on how bad it is
Whether you will definitely get covid depends on your—and everyone’s—assessment of how bad it would be to get. If the high end of possible long covid risks became clearly correct, probably many people wouldn’t take those costs vs. avoiding people who choose to be risky, so the options for low risk lifestyle would improve. Like, at first when people realized that it was potentially quite valuable to wash your hands after various bodily things, it would have been pretty annoying to be one of the few people trying to avoid contact with others so called ‘germs’. One might have resigned oneself to getting every disease contained in anyone’s bodily fluids. But eventually the idea of hand-washing being important has had enough traction that everyone can care a lot about other people washing their hands after using the bathroom say, and it imposes very little burden, because basically everyone has habits and infrastructure that make it easy to uphold hygiene.
If everyone believed that covid was bad enough to get, it would die out in a month (possibly with terrible economic downsides for a month). It probably isn’t that bad, but if it really is quite bad to get, and ways to avoid it exist, people will probably realize that eventually, and adjust.
Q. Getting covid later is probably better than earlier.
So far this trend seems strong: I would rather get covid now than in March 2020. I expect more of this, from better knowledge, medicine, vaccines, and availability of everything we already have.
If I expect to get covid every year for the next five years, adding one more bout now is adding one more especially bad bout in expectation.
R. Huge VOI in following behind the crowd, at a safe distance
I know many people resigning themselves to getting covid this month, and results so far suggest that a lot of them will indeed be infected.
If half of my friends are getting covid right now, there seems to be massive value in waiting another three months before reassessing precautions, so I can see how it goes for them. While noisy, I expect to get a better sense of the distribution of outcomes among people in my reference class—and especially whether there is a macroscopic chance of really dire outcomes—from this (I think regrettable) experiment than I get from cobbling together different studies about vaguely defined symptoms among ambiguous or not-quite-relevant demographics, with various guesstimated adjustments.
There also seems to be a huge amount of uncertainty about how bad long covid is. I and my friends have various intuitions and guesses about where assorted factors of two push in this direction or that, and I doubt any of us should be super confident that we are the one with the right intuitions and guesses.
I think waiting out this spike looks like the right move from a VOI perspective even if your own judgments come out in favor of long covid being probably fine. As long as you are decently uncertain—which it seems to me that you probably should be—there is a lot of information coming in (at least if you are someone in my social circles, but probably a lot of social circles are coming to have a lot more people with covid this month).
88 comments
Comments sorted by top scores.
comment by idle (idlenow) · 2022-01-19T01:41:21.670Z · LW(p) · GW(p)
I appreciate you describing brain fog as psychological torment.
I think most severe/life-disrupting cases of long COVID are indistinguishable from ME/CFS. (I think it would be correct to say long COVID "causes" ME/CFS.) As someone living with ME/CFS: yes, the cognitive dysfunction is torture. And pushing to do stuff anyway just makes things worse -- this is called post-exertional malaise.
The comparison to sleep deprivation is good, but I'll note that the brain fog I regularly experience due to ME/CFS is much worse than any sleep deprivation I had ever experienced in my life beforehand.
The cognitive dysfunction itself is awful. And the way it crushes your dreams is heartbreaking. Say goodbye to your career and all your intellectual interests.
(I mean, say goodbye to your interests in general. Your physical stamina gets wrecked too. I rarely have the physical stamina to cook simple meals without post-exertional malaise.)
The social isolation stemming from the mental fatigue is threefold:
1) I feel stupid when talking to my friends, because I kind of *am* stupid now. Especially in the context of real-time conversations. My memory and processing speed is not good.
2) When I try calling friends anyway, I am punished by post-exertional malaise afterwards. e.g. I spend the following day very uncomfortable and unable to function well enough to even distract myself. In this state, even watching simple TV can be uncomfortably exhausting.
3) My healthy friends just don't understand what it's like to be going through such a horrible illness. I feel boring. They don't know what to say. It works out to be very alienating and bad for mental health.
On top of all that, so many people don't believe this illness is "real" in some sense. They think it's just laziness, or aging, or psychological. (FWIW, my illness started at 23, and I saw multiple psychologists who concluded there was no plausible psychological basis for my illness.)
Imagine being psychologically tortured, socially isolated, and gaslit by a ton of people arguing that you aren't even sick. Potentially with no light at the end of the tunnel. It's extremely upsetting.
Lots of healthy people argue that lockdowns are bad for their mental health. I'd argue that ME/CFS is orders of magnitude worse -- even in my case, which is relatively mild. Up to you to decide if the risk is worth it in your case.
I've skimmed a lot of long COVID prevalence studies, and unfortunately, they often have huge sample biases and don't ask the right questions to track ME/CFS incidence. Overall, I agree with Scott's range of "a few tenths of a percent to a few percent" as the risk of really bad long COVID symptoms.
↑ comment by Sameerishere · 2022-02-20T00:57:07.318Z · LW(p) · GW(p)
So sorry to hear you're suffering through this, and thank you for sharing your experience!
comment by johnswentworth · 2022-01-16T17:42:46.860Z · LW(p) · GW(p)
This is not going to be kind, but it's true and necessary to state. I apologize in advance.
Had you asked me in advance, I would have said that Katja in particular is likely to buy into long covid even in a world where long covid is completely psychosomatic; I think you (Katja) are probably unusually prone to looking-for-reasons-to-"believe"-things-which-are-actually-psychosomatic, without symmetrically looking-for-reasons-to-"disbelieve".
On the object level: the "Long covid probably isn't psychosomatic" section of the post looks pretty compatible with that prior. That section basically says two things:
- Just because reports of long covid are basically uncorrelated with having had covid does not imply that long covid does not happen
- There is still evidence of higher-than-usual death rates among people who have had covid
If we take both of these as true, they point to a world where there are some real post-covid symptoms, but the large majority of reported long covid symptoms are still psychosomatic. That seems plausible, but for some reason it isn't propagated into the other sections of the post. For instance, the very first sections of this post are talking about anecdotes and survey studies (at least I think they're survey studies based on a quick glance, didn't look too close), and I do not see in any of those sections any warning along the lines of "BY THE WAY THE LARGE MAJORITY OF THIS IS PROBABLY PSYCHOSOMATIC". You're counting evidence which should have been screened off by the lack of correlation between self-reported long covid symptoms and actually having had covid.
Replies from: Siebe, KatjaGrace, MichaelStJules, steve2152, Siebe, MichaelStJules, jane-mccourt↑ comment by Siebe · 2022-01-17T13:51:08.200Z · LW(p) · GW(p)
That French study is bunk.
Seropositivity is NOT AT ALL a good indicator for having had covid: https://wwwnc.cdc.gov/eid/article/27/9/21-1042_article
It is entirely possible that all those patients who believe they had COVID are right.
Some researchers believe absence of antibodies after infection is positively correlated with long covid (I don't have a source).
This study is bunk and it's harmful for adequate treatment of seronegative patients. The psychosomatic narrative has been a lazy answer stifling solid scientific research into illnesses that are not well understood yet.
Replies from: johnswentworth, T3t, Zvi, EGI↑ comment by johnswentworth · 2022-01-17T16:28:43.595Z · LW(p) · GW(p)
Strong upvote, this is great info.
↑ comment by RobertM (T3t) · 2022-01-18T07:15:20.953Z · LW(p) · GW(p)
36% of our cohort represented serologic nonresponders
I don't see any way in which the results of the French study are incompatible with a 64% true positive rate on "did this person previously have covid". (Also, a 64% true positive rate is actually decent Bayesian evidence for having had covid, assuming a sufficiently large % of the underlying population has had covid, such that whatever the false positive rate is doesn't cause most/all of your positives to be false positives.)
↑ comment by Zvi · 2022-02-07T13:05:27.369Z · LW(p) · GW(p)
Writing up a Long Covid post and noticed this. Several things even taking study here at face value. Putting this here as a 'preprint' basically to see if there are counterarguments. And regardless, thanks for the link, it should be considered, but I do not think this constitutes bunk.
One, everyone with a Ct of about 25 or lower got antibodies, so we're talking about light cases or outright false positives that then didn't get antibodies. And the spike in cases of Ct~37 is weird enough that I suspect something wrong with the PCRs.
Two, this implies that positive antibody test still means Covid (no false positives, only false negatives) so it would take a VERY large correlation with long Covid to have no correlation show up in the final data - keep in mind that Ct<25 still meant full positives later, so the correlation here can't be that big.
Three, we'd basically have to assume that virus count isn't linked to chance of long Covid or this doesn't make any sense, because all the high virus count cases are getting positives anyway. But lots of virus seems like it would be more likely to lead to long Covid because physics?
Also from the French paper they use this source: https://pubmed.ncbi.nlm.nih.gov/33139419/ which reports tests have high accuracy and has >10x the sample size of the one linked above.
My interpretation of the linked study here is 'sufficiently mild cases sometimes don't generate antibodies but show up on PCR, and/or PCR tests are getting false positives and we should not take Ct>30 very seriously. E.g. from here.
7. What can CT values tell us? Samples with CT values <32 generally contain sufficient genetic material for WGS and are more likely to contain replication competent virus. Although there are limitations in the use of CT values, they are one factor to consider when evaluating molecular test results and can be useful in assessing the trend in the viral load. If there is high suspicion of a new infection, laboratories may attempt WGS on samples with CT value <32.
The bulk of the issues were in CT values >=32.
Anyone have more thoughts?
↑ comment by EGI · 2022-03-02T20:31:02.223Z · LW(p) · GW(p)
Same problem as with Lyme Disease. Weak or no antibody reaction is only good news IF it indicates absence of the pathogene. While this is not unreasonable to assume, it still needs to be demonstrated, preferably over a wide variety of differen tissues.
↑ comment by KatjaGrace · 2022-01-16T23:22:39.590Z · LW(p) · GW(p)
I agree that I'm more likely to be concerned about in-fact-psychosomatic things than average, and on the outside view, thus probably biased in that direction in interpreting evidence. Sorry if that colors the set of considerations that seem interesting to me. (I didn't mean to claim that this was an unbiased list, sorry if I implied it. )
Some points regarding the object level:
- The scenario I described was to illustrate a logical point (that the initially tempting inference from that study wasn't valid). So I wouldn't want to take the numbers from that hypothetical scenario and apply them across the board to interpreting other data. I haven't thought through what range of possible numbers is really implied, or whether there are other ways to make sense of these prima facie weird findings (especially re lack of connection between having covid and thinking you have covid). If I put a lot of stock in that study, I agree there is some adjustment to be made to other numbers (and probably anyway - surely some amount of misattribution is going on, and even some amount of psychosomatic illness).
- My description was actually of how you would get those results if approximately none of the illness was psychosomatic but a lot of it was other illnesses (the description would work with psychosomatic illnesses too, but I worry that you misread my point, since you are saying that in that world most things are psychosomatic, and my point was that you can't infer that anything was psychosomatic).
- If the scenario I described was correct, the rates of misattribution implied would be specific to that population and their total ignorance about whether they had covid, rather than a fact intrinsic to covid in general, and applicable to all times and places. I do find it very hard to believe that in general there is not some decently strong association between having covid and thinking you have covid, even if also a lot of errors.
- It's a single study, and single studies find all kinds of things. I don't recall seeing other evidence supporting it. In such a case, I'm inclined to treat it as worthy of adding some uncertainty, but not worthy of a huge update about everything.
- If this consideration reduced real long covid cases by a factor of two, it doesn't feel like that changes the story very much (there's a lot of factor-of-two-level uncertainty all over the place, especially in guessing what the rate is for a specific demographic), so I guess it doesn't seem cruxy enough to give a lot of attention to.
- I agree that mostly it isn't salient to me that some fraction of cases are misattributions, and that maybe I should keep it in mind more, and say things like 'it looks like many people who think they had covid can no longer do their jobs' instead of taking things at face value. Though in my defense, this was a list of considerations, so I'm also not flagging all of the other corrections one might want to make to numbers throughout, as I might if I were doing a careful calculation.
- It's true that I don't really believe that half of the bad cases at least are misattributions or psychosomatic—the psychosomatic story seems particularly far-fetched (particularly for the bad cases). Perhaps I'm mis-imagining what this would look like. Is there other evidence for this that you are moved by?
↑ comment by johnswentworth · 2022-01-17T00:31:23.000Z · LW(p) · GW(p)
Good points. Some responses:
- I put a lot more trust in a single study with ground-truth data than in a giant pile of studies with data which is confounded in various ways. So, I trust the study with the antibody tests more than I'd trust basically-any number of studies relying on self-reports. (A different-but-similar application of this principle: I trust the Boston wastewater data on covid prevalence more than I trust all of the data from test results combined.)
- I probably do have relatively high prior (compared to other people) on health-issues-in-general being psychosomatic. The effectiveness of placebos (though debatable) is one relevant piece of evidence here, though a lot of my belief is driven by less legible evidence than that.
- I expect some combination of misattribution, psychosomaticity, selection effects (e.g. looking at people hospitalized and thereby accidentally selecting for elderly people), and maybe similar issues which I'm not thinking of at the moment to account for an awful lot of the "long covid" from self-report survey studies. I'm thinking less like 50% of it, and more like 90%+. Basically, when someone runs a survey and publishes data from it, I expect the results to mostly measure things other than what the authors think they're measuring, most of the time, especially when an attribution of causality is involved.
↑ comment by Adele Lopez (adele-lopez-1) · 2022-01-19T01:15:04.516Z · LW(p) · GW(p)
Even if long covid is entirely psychosomatic, it's worth avoiding those psychosomatic effects. One way to avoid them is to debunk (potentially at the gut intuition level, which is harder to reliably do) non-psychosomatic causes of it. Another way is to avoid covid in the first place. I expect the most effective strategy will include some combination of these.
I see "psychosomatic" often used as a semantic stopsign [LW · GW]. Once something is called "psychosomatic", people typically stop trying to figure out a way to solve the problem. I don't know of any reliable and credible ways to resolve psychosomatic issues, it's mostly meditation guys and alternative medicine quacks who even try.
If it's really true that a large amount of health-issues-in-general are psychosomatic, then that's a really huge problem which we don't have an adequate solution for! (I expect that you agree with this, I just am trying to push against the weight of the semantic stopsign that people have around this concept.)
↑ comment by ChristianKl · 2022-01-17T17:32:58.900Z · LW(p) · GW(p)
Psychosomatic is a word that's gets often used as if that would mean that illnesses aren't real.
If you tell someone with an allergy to cats to imagine that they are stocking a cat, that can be enough to trigger the allergy symptoms. The fact that an imagined cat is good enough to trigger the allergy shows quite clearly that the allergy is partly psychosomatic as it can be triggered psychologically.
The underlying mechanisms of such an immune response are however deep. One model of long COVID is, that it's partly about autoimmune issues. Those might be as psychosomatic as the above example of cat allergy. There's a neuronal pattern that gets the body to trigger defenses in a misaligned way.
↑ comment by MichaelStJules · 2022-01-16T18:38:24.295Z · LW(p) · GW(p)
I would be surprised if the worst cases, where people can't really work and it lasts about half a year or longer, were mostly psychosomatic, or at least mostly psychosomatic in a way that's easily avoidable by just having different beliefs about long COVID. Can you really believe yourself into debilitating chronic fatigue and brain fog for half a year?
(EDITED: "a year -> "half a year", since I don't recall long COVID studies going much longer than half a year, when I looked into them, which was probably 3-6 months ago.)
Replies from: pktechgirl↑ comment by Elizabeth (pktechgirl) · 2022-01-16T20:49:37.470Z · LW(p) · GW(p)
I broadly agree but don't think that proves covid was the culprit. Vague shitty symptoms doctors refuse to grapple with were a problem long before covid, and if people with these symptoms can get better care by calling it long covid than leaving it open or blaming something else, they'd be stupid not to.
Replies from: MichaelStJules↑ comment by MichaelStJules · 2022-01-16T20:58:18.576Z · LW(p) · GW(p)
That's a good point. I think the comparison of severe symptoms between COVID-positive COVID-negative matched controls would be good evidence about the risk. I don't recall if any comparison studies tracked severity between positive and matched negative groups, though, rather than mostly just presence of symptoms, and I do recall studies without comparisons tracking severity, which people could use to report non-COVID-related severe symptoms, as you suggest.
Replies from: pktechgirl↑ comment by Elizabeth (pktechgirl) · 2022-01-17T06:58:58.032Z · LW(p) · GW(p)
When I looked into this there was a paper that compared psych sequelae from covid to influenza and flu-like illnesses and found "covid to be modestly worse except for myoneural junction and other muscular diseases, where covid 5xed the risk (although it’s still quite low in absolute terms). Dementia risk is also doubled, presumably mostly among the elderly." This was not controlling for age or acute severity, and data was gathered pre-vaccine.
(note: I did this research months ago and haven't done any follow-up, so trust what I wrote then over what I remember now)
↑ comment by Steven Byrnes (steve2152) · 2022-01-16T18:00:16.980Z · LW(p) · GW(p)
My impression from here [LW · GW] is that "reports of long covid are basically uncorrelated with having had covid" is a misunderstanding of the French study.
Replies from: johnswentworth↑ comment by johnswentworth · 2022-01-16T18:08:24.549Z · LW(p) · GW(p)
Good point. If we take that post's analysis at face value, then a majority of reported long covid symptoms are probably psychosomatic, but only just barely a majority, not a large majority. Though looking at the post, I'd say a more accurate description is that at least a majority of long covid symptoms are psychosomatic, i.e. it's a majority even if we pretend that all of the supposedly-long-covid symptoms in people who actually had covid are "real".
Replies from: Lanrian↑ comment by Lukas Finnveden (Lanrian) · 2022-01-17T06:27:01.944Z · LW(p) · GW(p)
Why does the post imply that a majority of long covid symptoms are psychosomatic?
Let's say covid is entirely non-psychosomatic, and that we have the following groups:
(0) People who never had covid, never thought they had covid.
(1) People with asymptomatic covid, who don't believe they had covid.
(2) People with noticeable covid, no long covid.
(3) People with noticeable covid, including long covid.
(4) People who mistake something short-term (like a cold) for covid.
(5) People who have some serious long-term issues, that they mistake for long covid.
Now we have three variables:
(a) Antibody group = (1) + (2) + (3)
(b) Belief-in-covid = (2) + (3) + (4) + (5)
(c) Claimed long covid = (3) + (5)
If group (4) is relatively small and/or group (1) is relatively large and/or group (5) is relatively large, then it makes sense that (b) is a way better predictor for (c) than (a) is.
The french study found that (a) isn't a good predictor for (c) if you control for (b). I don't have a good enough intuition for regression with multiple variables to know whether this is unsurprising given the previous paragraph; but my guess is that this is unsurprising given the previous paragraph.
Replies from: johnswentworth↑ comment by johnswentworth · 2022-01-17T18:14:00.321Z · LW(p) · GW(p)
Sorry, I was lumping together misattribution and the like under "psychosomaticity", and I probably shouldn't have done that.
Replies from: Lanrian↑ comment by Lukas Finnveden (Lanrian) · 2022-01-18T03:53:08.776Z · LW(p) · GW(p)
I still don't see how you can know that the majority of long covid is misattribution and the like. If (1) is large, and (4) + (5) are both negligibly small, then belief-in-covid will be a better predictor of long covid just because symptomatic covid is a better predictor of long covid than asymptomatic+symptomatic covid is.
↑ comment by Siebe · 2022-01-17T16:12:44.832Z · LW(p) · GW(p)
In addition, we know that 100% of patients with long COVID have microclots, at least in this study: https://www.researchsquare.com/article/rs-1205453/v1
Interestingly, they diagnosed patients not via PCR or antibodies, but based on exclusion and symptom diagnosis:
"Patients gave consent to study their blood samples, following clinical examination and/or after filling in the South African Long COVID/PASC registry. Symptoms must have been new and persistent symptoms noted after acute COVID-19. Initial patient diagnosis was the end result of exclusions, only after all other pathologies had been excluded. This was done by taking a history of previous symptoms (before and after acute COVID- 19 infection), clinical examinations, and investigations including: full blood counts; N-terminal pro b-type natriuretic peptide (NTproBNP) levels (if raised it suggests cardiac damage); thyroid-stimulating 7 hormone (TSH); C-reactive protein levels; the ratio between the concentrations of the enzymes aspartate transaminase and alanine transaminase (AST/ALT ratio) andelectrocardiogram (ECG) +/- stress testing. If the mentioned tests were in the normal ranges, the lingering symptoms that can be ascribed to Long COVID/PASC were then assessed and included shortness of breath; recurring chest pain; lingering low oxygen levels; heart rate dysfunction (heart palpitations); constant fatigue (more than usual); joint and muscle pain; brain fog; lack of concentration; forgetfulness; sleep disturbances and digestive and kidney problems. These symptoms should have been persistent and new symptoms that were not present before acute COVID-19 infection and persistent for at least two months after recovery from acute (infective) COVID-19." (P. 6-7)
I'd say this should be convincing evidence that as good as none of the patients that claim to have long covid have a psychosomatic issue. It's not like microclots are a common and harmless issue either.
Replies from: johnswentworth↑ comment by johnswentworth · 2022-01-17T17:28:54.890Z · LW(p) · GW(p)
This mostly sounds like age-related problems. I do expect generic age-related pathologies to be accelerated by covid (or any other major stressor), but if that's the bulk of what's going on, then I'd say "long covid" is a mischaracterization. It wouldn't be relevant to non-elderly people, and to elderly people it would be effectively the same as any other serious stressor.
Replies from: Siebe, florin-clapa↑ comment by Siebe · 2022-01-18T11:42:08.110Z · LW(p) · GW(p)
No, these problems are most probably cause by a lack of oxygen getting through to tissues. There's a large amount of patients reporting these severe symptoms in patients groups, and they're not elderly.
It honestly feels to me like you really want to believe long COVID isn't a big deal somehow.
Replies from: johnswentworth↑ comment by johnswentworth · 2022-01-18T17:25:54.485Z · LW(p) · GW(p)
It's not that I don't want to believe it, it's that long covid is the sort of thing I'd expect to hear people talk about and publish papers about even in a world where it isn't actually significant, and many of those papers would have statistically-significant positive results even in a world where long covid isn't actually significant. Long covid is a story which has too much memetic fitness independent of its truth value. So I have to apply enough skepticism that I wouldn't believe it in a world where it isn't actually significant.
No, these problems are most probably cause by a lack of oxygen getting through to tissues.
That sounds right for shortness of breath, chest pain, and low oxygen levels. I'm more skeptical that it's driving palpitations, fatigue, joint and muscle pain, brain fog, lack of concentration, forgetfulness, sleep disturbance, and digestive and kidney problems; those sound a lot more like a list of old-age issues.
Replies from: Siebe↑ comment by Siebe · 2022-01-18T20:22:50.796Z · LW(p) · GW(p)
See figure 2 of this large scale survey: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/7october2021
"As a proportion of the UK population, prevalence of self-reported long COVID was greatest in people aged 35 to 69 years, females, people living in more deprived areas, those working in health or social care, and those with another activity-limiting health condition or disability"
↑ comment by Florin (florin-clapa) · 2022-01-17T22:14:53.654Z · LW(p) · GW(p)
Covid is airborne aging via SARS-CoV-2-induced senescent cell development.
Even non-elderly people might age faster, especially if they're overweight or obese.
↑ comment by johnswentworth · 2022-01-17T22:53:16.177Z · LW(p) · GW(p)
That is not how senescent cells work. They turn over on a fast timescale. If covid induces a bunch of senescent cell development (which indeed makes sense), those senescent cells should generally be cleared out on a timescale of weeks. Any long-term effects would need to be mediated by something else.
Replies from: florin-clapa↑ comment by Florin (florin-clapa) · 2022-01-17T23:54:39.086Z · LW(p) · GW(p)
But some of those SnCs probably won't be cleared, and that extra burden of SnCs (especially if it's much higher than what intrinsic aging produces during a short period of time) might be what's causing long covid.
Replies from: johnswentworth↑ comment by johnswentworth · 2022-01-18T00:06:12.780Z · LW(p) · GW(p)
At this point, I have yet to see any compelling evidence that any SnCs stick around over a long timescale, despite this being a thing which I'd expect to have heard about if anybody had the evidence. Conversely, it sure does look like treatments to remove senescent cells have to be continuously administered; a one-time treatment wears off on roughly the same timescale that SnCs turn over. That pretty strongly suggests that there are not pools of long-lived SnCs hanging around. And a noticeable pathology would take a lot of SnCs sticking around.
Replies from: florin-clapa↑ comment by Florin (florin-clapa) · 2022-01-18T01:11:44.072Z · LW(p) · GW(p)
The paper you linked to seems to claim that SnCs do stick around.
In old mice, baseline SnC levels are about 5-fold higher, and SnC removal rate is slower than in young mice (p=0.038).
This suggests that middle-aged mice should also have some baseline SnC level, although perhaps not as much as old mice. Also, the level of SnCs didn't return to baseline in the old mice even at the 40 day mark.
Replies from: johnswentworth↑ comment by johnswentworth · 2022-01-18T01:31:49.722Z · LW(p) · GW(p)
"Baseline" does not mean they stick around. It means that background processes introduce new SnCs at a steady rate, so the equilibrium level is nonzero. As the removal rate slows, that equilibrium level increases, but that still does not mean that the "baseline" SnCs are long-lived, or that a sudden influx of new SnCs (from e.g. covid) will result in a permanently higher level.
Replies from: florin-clapa↑ comment by Florin (florin-clapa) · 2022-01-18T02:05:20.370Z · LW(p) · GW(p)
Even if the original SnCs are eventually eliminated (which isn't entirely clear), it sure looks like they should increase the SnC baseline anyway. It's not just background processes that can produce new SnCs, but SnCs themselves produce new, secondary SnCs too. So, it's not unlikely that adding a bunch of SnCs to the baseline pool of SnCs (whose size increases with age) could further increase the size of this pool. And that would be a net increase in biological age.
This might not be a problem for young mice which can eliminate SnCs fairly quickly, but it seems to be a big problem for old mice. Middle-aged mice probably lie somewhere in between. I'd also expect that overweight, obese, or otherwise messed-up, middle-aged mice would fare worse.
Replies from: tailcalled↑ comment by tailcalled · 2022-01-19T20:49:34.885Z · LW(p) · GW(p)
It's not just background processes that can produce new SnCs, but SnCs themselves produce new, secondary SnCs too.
Imagine that each new SnC produced 3 new SnCs within a day, and also that SnCs had a 50% chance of being removed each day. In that case, there will be 4*0.5 = 2x as many SnCs tomorrow as there is today, leading to exponential runaway growth, immediately exploding in the number of SnCs and dying.
On the other hand, imagine that they only produce 1 new SnC within a day, and also that they had a 66% chance of being removed each day. In that case there will be 2*0.33 = 0.66x as many SnCs tomorrow, leading to quickly returning to the equillibrium caused by outside production.
You'd need some sort of fine-tuning where the production and removal are extremely close to each other to not either have explosive growth or rapid equillibration.
↑ comment by Elizabeth (pktechgirl) · 2022-01-17T22:25:45.847Z · LW(p) · GW(p)
How does this compare to other contagious diseases?
EDIT: for aging in particular.
↑ comment by Florin (florin-clapa) · 2022-01-18T22:46:14.037Z · LW(p) · GW(p)
It's probably too early to compare the amount of senescence that's produced by SARS-CoV-2 versus other viruses, but what is known is that several viruses (including influenza) do induce the development of senescent cells in several tissues.
Replies from: pktechgirl↑ comment by Elizabeth (pktechgirl) · 2022-01-18T23:07:55.377Z · LW(p) · GW(p)
Then this doesn't seem like a counterargument to "to elderly people it would be effectively the same as any other serious stressor" to me.
Replies from: florin-clapa↑ comment by Florin (florin-clapa) · 2022-01-19T03:23:42.937Z · LW(p) · GW(p)
The counterargument would apply to "It wouldn't be relevant to non-elderly people...."
Replies from: pktechgirl↑ comment by Elizabeth (pktechgirl) · 2022-01-19T05:23:54.309Z · LW(p) · GW(p)
Ah, yes. I think young people should probably take the long term effects of viruses more seriously in general.
Replies from: florin-clapa↑ comment by Florin (florin-clapa) · 2022-01-19T20:36:49.963Z · LW(p) · GW(p)
I'd say that unhealthy-for-their-age young and middle-aged people and otherwise healthy-but-middle-aged people might want to be more cautious. Healthy-for-their-age young people probably don't need to worry.
↑ comment by MichaelStJules · 2022-01-16T20:28:15.427Z · LW(p) · GW(p)
For what it's worth, I agree that the post reads to me as not very balanced, but a lot of the evidence and arguments presented are still worrying, and I am still worried about long COVID. (I also don't put myself above confirmation bias, though.)
G. Overall deaths from everything have been very unusually high at points in 2021, even in 15-64 age group
This could also be explained by things other than COVID or long COVID, too, e.g. lockdown/isolation, less exercise, increased depression, poorer access to healthcare.
↑ comment by Heron (jane-mccourt) · 2022-01-16T20:57:32.528Z · LW(p) · GW(p)
Sure it is essential to differentiate between those who have been tested for COVID and that self-reporting which, in the absence of a test, is another information source. To repeat my experience of becoming ill in the time of COVID 19: I couldn't get a test in July 2020; I don't know whether it was COVID-19 that hit me like a speeding train. I still have cognitive difficulties, severe fatigue, continuous headaches, lack of taste and smell, and other new things which have gone wrong physically. I'm waiting for the latest results of brain/spine MRI; I'm without a diagnosis. My reading suggests M.E., encephalitis, Long COVID and possibly lots of things - continued testing thus far provides no answer. I've also learned about FND and can see how these symptoms could, in the absence of an actual biomarker, be put under that umbrella. To have one's symptoms acknowledged matters. Losing one's fundamental abilities to function is so devastating; reading that such symptom clusters are deemed psychosomatic seems, to the afflicted, unhelpful.
comment by Randomized, Controlled (BossSleepy) · 2022-01-16T16:54:16.901Z · LW(p) · GW(p)
Thank you for this. I'd say prior to reading this I was around 70% that for someone recently vaccinated or boosted Omicron isn't really worth worrying about, and getting Omicron at some point might even be +EV, due to cross immunity effect [LW · GW]. I'd say now I'm around.. 45% on this?
My sense is that EAs in general have not been in the "strict lockdown" mode, trying to do some more careful tradeoffs to allow for things like EAGs. This struck me as.. reasonable-ish at the time, (even up through delta). But if Omicron has a similar long-covid story, this suggests that the upcoming EAGs may not be a good idea in person.
comment by Steven Byrnes (steve2152) · 2022-01-16T12:51:03.831Z · LW(p) · GW(p)
For the (K) "belief in having had long COVID" (psychosomatic) French study thing see also https://www.lesswrong.com/posts/LETXrTsGAqJrcik3T/french-long-covid-study-belief-vs-infection [LW · GW]
comment by Ruby · 2022-01-16T22:32:57.685Z · LW(p) · GW(p)
Frontpaging this despite the current policy to leave most Covid content on Personal Blog. Doing so because it is of interest and broad relevance to people's decisions and seems high-effort and high-quality, though note questioning of biased reasoning in the comments.
comment by MichaelStJules · 2022-01-16T20:40:26.122Z · LW(p) · GW(p)
Q. Getting covid later is probably better than earlier.
As a counter consideration, vaccine effectiveness might wane quickly, and it's likely better to get COVID while better protected than while less protected. See, e.g. https://www.webmd.com/vaccines/covid-19-vaccine/news/20211227/covid-booster-protection-wanes-new-data
That being said, I'm still leaning towards avoiding COVID to avoid long COVID.
comment by MichaelStJules · 2022-01-18T06:08:51.306Z · LW(p) · GW(p)
I think we should look further into this study, which seems somewhat reassuring, but I have reservations about it:
Kuodi et al., January 2022, "Association between vaccination status and reported incidence of post-acute COVID-19 symptoms in Israel: a cross-sectional study of patients tested between March 2020 and November 2021" (pdf, not yet peer-reviewed)
Their previous version understated the results, since it didn't include the uninfected. The new version does, and says (cutting out some text before and after, and emphasis added by me):
Methods: We invited individuals who were PCR tested for SARS-CoV-2 infection at participating hospitals between March 2020-November 2021 to fill an online questionnaire that included baseline demographics, details of their acute episode and information about symptoms they were currently experiencing. Using binomial regression, we compared vaccinated individuals with those unvaccinated and those uninfected in terms of self-reported symptoms post-acute infection.
Results: We included 951 infected and 2437 uninfected individuals. Of the infected, 637(67%) were vaccinated. The most commonly reported symptoms were; fatigue (22%), headache (20%), weakness (13%), and persistent muscle pain (10%). After adjusting for follow-up time and baseline symptoms, those who received two doses less likely than unvaccinated individuals to report any of these symptoms by 64%, 54%, 57%, and 68% respectively, (Risk ratios 0.36, 0.46, 0.43, 0.32, p<0.04 in the listed sequence). Those who received two doses were no more likely to report any of these symptoms than individuals reporting no previous SARS-CoV-2 infection.
Conclusions: Vaccination with at least two doses of COVID-19 vaccine was associated with a substantial decrease in reporting the most common post-acute COVID-19 symptoms, bringing it back to baseline. Our results suggest that, in addition to reducing the risk of acute illness, COVID-19 vaccination may have a protective effect against long COVID.
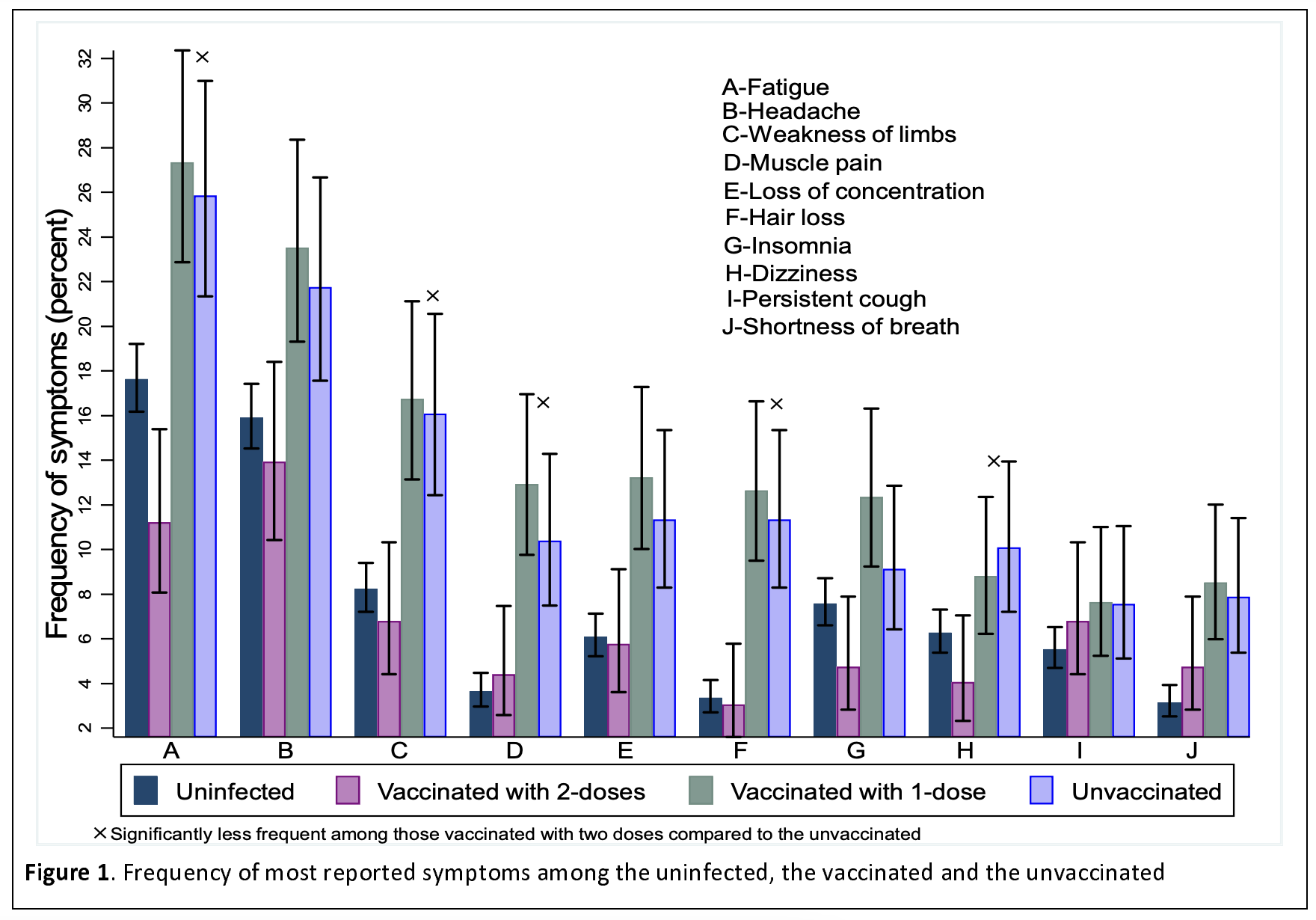
One thing that's pretty suspicious here and could cast doubt on these results is that the uninfected were more likely than the infected doubly vaccinated to have some of these long COVID symptoms, including the most common one, fatigue (and that seems to be the only one for which there's a statistically significant difference, driven by those aged 36+).
On what they did:
A first series of binomial regression models were fitted to the data for the ten most commonly reported post-COVID-19 symptoms according to vaccination status. We adjusted for the difference in follow-up time and proportion of asymptomatic patients at the time of diagnosis between the groups. We then compared vaccinated and infected individuals to never infected individuals in terms of reported symptoms, also using binomial regression models. We used two distinct steps since it was not possible to adjust for follow-up time and symptoms at baseline among uninfected patients.
To take the anticipated age differences into account, the analysis was age-stratified and differences in the length of time from the beginning of symptoms to responding to the survey were adjusted for in the model. Vaccination status was recorded as either one dose or two doses. At the time of data collection, very few individuals had received a third dose and those who did were recorded as two doses.
It's not clear to me whether or not they adjusted for the demographic characteristics they collected (summarized in table 1).
Some possible explanations and potential weaknesses of the study:
1. The sample sizes are not very large, so it could be noisy. They only had 59, 135 and 100 doubly vaccinated + infected individuals in the 19-35, 36-60 and >60 age groups, respectively. The number of uninfected was much larger, though, 2437 together. As far as I can tell, they didn't make any adjustments for multiple comparison tests, and they did >160 tests, for the different symptoms and age groups.
2. I don't know if they made any adjustments (other than age stratification) for the comparisons to the Uninfected group, and this could leave bias. If they did make any such adjustments, they might not have made enough. They didn't do any matching.
There could be group differences not accounted for that would bias it this way, e.g. people who got vaccinated and infected could have been more health-conscious on average than those who were uninfected (with any vaccination status). We might think the uninfected are demographically between the unvaccinated+infected and vaccinated+infected. Compared to the unvaccinated+infected, the doubly vaccinated+infected were more likely to have tertiary education (62.9% vs 52.1%), more likely to have hypertension (13.9% vs 5.1%) and more likely to have diabetes (8.2% vs 3.8%). Hypertension and diabetes should point to the opposite bias, though, if unadjusted for. (I think it's unlikely they adjusted for anything they should not have adjusted for in a way that increased bias, although such adjustments can increase variance.)
3. Some of those considered uninfected could actually have been infected, and ended up with long COVID. They used "uninfected in terms of self-reported symptoms post-acute infection", but it's possible some asymptomatic infected individuals get long COVID, and some of these asymptomatic infected individuals were probably not vaccinated. Their positive cases were based on "self-reported positive PCR results".
4.The vaccines could protect against long COVID-like symptoms from other causes. Maybe through the placebo effect?
Overall, given how large the gap is between uninfected and doubly vaccinated+infected, and the reasonable assumption that vaccination + infection should actually be worse than never getting infected, that gap could easily hide a risk of long COVID of around 1% (at least for fatigue).
comment by Richard Korzekwa (Grothor) · 2022-01-17T20:35:52.495Z · LW(p) · GW(p)
If half of my friends are getting covid right now, there seems to be massive value in waiting another three months before reassessing precautions, so I can see how it goes for them. While noisy, I expect to get a better sense of the distribution of outcomes among people in my reference class—and especially whether there is a macroscopic chance of really dire outcomes—from this (I think regrettable) experiment than I get from cobbling together different studies about vaguely defined symptoms among ambiguous or not-quite-relevant demographics, with various guesstimated adjustments.
I recommend registering in advance how you will evaluate the new information you get over the next several months. In particular, it would be valuable to write down your credence on various outcomes, conditional on covid being something that is worth paying a substantial cost to avoid.
My guess is that you and I will disagree on what we're likely to see in low vs high risk worlds. For example, I think that A and B in your analysis are almost guaranteed, whether long covid risk is large or small. Also, C, F, G, H, and L are entirely consistent with low risk, and only modestly more likely in worlds where long covid is a major concern.
comment by MichaelStJules · 2022-01-16T17:39:03.883Z · LW(p) · GW(p)
EDIT: I forgot (or didn't know) that loss of sense of smell was less likely with Omicron, which Steven Byrnes pointed out. Seems like 12-20% (probably mostly vaccinated?) of Omicron infections vs 7-68% for previous variants (section 3.5, and I'm not sure to what extent vaccination status was considered here). I've also read that Delta was less likely to cause loss of sense of smell than earlier variants, too. If the probability of loss of sense of smell scales proportionally with other brain issues, then I'd guess Omicron is less severe than previous variants (assuming 2 doses of mRNA vaccines against Delta, and 3 against Omicron, with the last one recently). Maybe by a factor of ~2x, which is somewhat but not extremely reassuring.
Also, it's not clear that long COVID is less bad or less likely with Omicron than Delta (for a fully vaccinated person). IIRC, vaccines are less effective at reducing symptoms even conditional on catching COVID, and the supposed mildness of Omicron might be explained by which part of the respiratory system it attacks, but that might not have much bearing on how it affects the nervous system and brain in particular (if it does). Brain fog and chronic fatigue seem more like brain issues than respiratory issues, although maybe poor breathing could cause both?
There are studies for and against COVID infecting the brain (I haven't taken the time to evaluate them), and in particular olfactory regions, which could explain long term loss of smell. If it does have a route to the brain, that's very worrying and would likely rule out a purely psychosomatic explanation (although both could be involved), although I agree that the severity of some cases, the specificity of some symptoms, and long COVID progression (IIRC, it can have a fairly delayed onset) make a purely psychosomatic explanation unlikely already.
EDIT: Here are a few studies, but I wouldn't consider this a particularly representative sample, and again, I haven't looked through them in much detail.
For brain route:
- Song et al., January 2021, Neuroinvasion of SARS-CoV-2 in human and mouse brain
- Douaud et al., August 2021, Brain imaging before and after COVID-19 in UK Biobank (not yet peer-reviewed)
Against brain route:
Replies from: steve2152↑ comment by Steven Byrnes (steve2152) · 2022-01-16T17:53:22.832Z · LW(p) · GW(p)
I thought omicron didn't cause as much loss of sense of smell as previous strains? I was thinking of that (very tentatively) as a good sign, like "omicron is less of a destroyer of nerve cells", and I think of nerve cells as being unusually difficult to heal, cf. polio. (Omicron does cause brain fog, which is bad but not necessarily associated with the killing of nerve cells, or at least that's my vague impression / guess.) Low confidence on all this.
Replies from: MichaelStJules↑ comment by MichaelStJules · 2022-01-16T18:20:15.996Z · LW(p) · GW(p)
I thought omicron didn't cause as much loss of sense of smell as previous strains?
Hmm, ya, that seems right. From a quick Google search: https://www.businessinsider.com/loss-of-taste-smell-not-common-covid-symptoms-2022-1.
Maybe Omicron just doesn't get as deep in the body generally, too, then. That would be a good sign, too.
comment by [deleted] · 2022-01-18T19:23:40.071Z · LW(p) · GW(p)
Thanks for such a thorough post. I'm basically trying to figure out if all this evidence holds when you have received a booster and what is the evidence for that. One question: for all the studies that you shared showing long covid negative impacts, what is the percentage of those studies that focus on getting COVID-19 (a) without vaccines (b) with "initial" vaccines (c) with a booster? Eg maybe 20% of the studies are about assessing the impact of COVID when you haven't received any vaccines, while 30% is about assessing the impact of COVID when you got the "initial" vaccines, and 50% all combined or something like that. I'd be curious about your rough assessment given that I'm sure this may take too long to do very much in detail.
Replies from: Grothor↑ comment by Richard Korzekwa (Grothor) · 2022-01-19T02:33:18.235Z · LW(p) · GW(p)
There's the study mentioned in another comment [LW · GW] that shows promising-but-suspicious evidence that vaccines more-or-less eliminate long covid risk.
Katja may be able to tell you if she knows more about the particular studies she cites, but I've found that there is very little good research on long covid that is not mostly or entirely looking at unvaccinated cases. The Norwegian pre-print that Katja mentions explicitly excludes vaccinated people. I don't see stats on the dates for the papers in the 81 study review article she cites, nor did I look at the dates on all 81 studies, but I did look at the ones with controls and they were all from 2020 or the first half of 2021, so pretty clearly too early to look at vaccinated covid. All of the high-quality studies I'm aware of are too early to include any substantial number of vaccinated cases.
This is unfortunate and somewhat preventable, but not too surprising. There were not many breakthrough cases before the delta waves, which didn't take off until about 7 months ago. This doesn't leave much time for researchers to track people who recover from acute cases and show months of persistent symptoms, then write a paper and get it published.
comment by MichaelStJules · 2022-01-16T22:40:46.556Z · LW(p) · GW(p)
One major concern I have with the tail of long COVID is its severity even if/when it does get better after a few years. If I have debilitating long COVID for 3 years and then I recover fully, how will my career be affected, and what kind of person will I be after that? I think it's reasonably likely that it would cause value drift away from effective altruism (in part because being connected to EA while feeling hopeless about my own future productivity seems psychologically painful, and if I become primarily preoccupied with my own recovery and wellbeing), so under my current values, a 3-year case of debilitating long COVID could cost me about half of my expected future altruistic value, which would be like a ~50% chance of my own death. My inside view, just considering my own psychology and ignoring external evidence of value drift, is that I would very likely get back to EA.
Getting COVID once seems like an around 0.2%-2% chance of something at least this bad for me (based primarily on Matt Bell's analysis for the high end, with downward adjustments for my good health, Omicron being less severe, and concerns about study bias for severity for the lower end). This is bad enough to me to worry about, but also not so bad that I'm not willing to make tradeoffs for exercise, mental health and productivity generally, based on gathering size, vaccine effectiveness and local case counts, etc.. It's mild enough that new information seems reasonably likely to update me towards no longer worrying about long COVID, and most of the considerations I've come across not accounted for in Matt Bell's analysis seem to point towards less severe. However, it's also not clear to me that each time you get COVID is less bad in expectation than earlier times, since immunity wanes, and you will be older and potentially accumulate more harms from COVID, increasing its severity when it does reinfect you.
For those working on short timeline-focused AI safety, long COVID could cost you most of your chance to contribute.
I think I would very likely get back to EA with only about 1 year of long COVID or less. I also think there's substantial probability that I'd get back to EA no matter how long before I'm mostly recovered, as long as I do recover, at least 20%.
As an aside, naively, psychedelics seem promising as a treatment for brain fog and chronic fatigue from long COVID (whether or not it's psychosomatic).
comment by MichaelStJules · 2022-03-07T05:57:34.262Z · LW(p) · GW(p)
There's a new preprint with what seem to be good controls, although based on self-report and the participation rate was low, about 1/3:
Post-acute symptoms, new onset diagnoses and health problems 6 to 12 months after SARS-CoV-2 infection: a nationwide questionnaire study in the adult Danish population
Anna Irene Vedel Sørensen, Lampros Spiliopoulos, Peter Bager, Nete Munk Nielsen, Jørgen Vinsløv Hansen, Anders Koch, Inger Kristine Meder, Steen Ethelberg, Anders Hviid
medRxiv 2022.02.27.22271328; doi: https://doi.org/10.1101/2022.02.27.22271328
Methods We conducted a nationwide cross-sectional study including 152 880 individuals aged 15-years or older, consisting of RT-PCR confirmed SARS-CoV-2 cases between September 2020-April 2021 (N=61 002) and a corresponding test-negative control group (N=91 878). Data were collected 6, 9 or 12 months after the test using web-based questionnaires. The questionnaire covered acute and post-acute symptoms, selected diagnoses, sick leave and general health, together with demographics and life style at baseline. Risk differences (RDs) between test-positives and -negatives were reported, adjusted for age, sex, single comorbidities, Charlson comorbidity score, obesity and healthcare-occupation.
I recommend checking out the figures for risk differences for new self-reported health problems and new self-reported diagnoses. From figure 2, the risk difference for a new self-reported diagnosis of chronic fatigue syndrome (pooled across groups) was 2.5%=4%-1.5%, the largest of the diagnoses and statistically significant. 1.15% for anxiety, 1% for depression, 0.16% for PTSD and a non-statistically significant difference for fibromyalgia. From figure 3, the risk differences for new health problems they tested were pretty big, 17.27% (sleep problems) to 40.45% (physical exhaustion).
Figure 4 has risk differences for various health conditions by age group and gender, but not necessarily for new onset since COVID.
They highlight self-report and participation rates as the main limitations:
The main limitations of the study are the self-reporting of symptoms and the participation rate. With little over 1/3 of the invitees choosing to participate, we cannot rule out participation bias. The motivation for participation could be higher among those experiencing post-acute symptoms, but on the other hand, those with very severe symptoms might not have had the energy to participate. Still, response rates among test-positives and –negatives were similar. However, because of the size of the study and the marked risk differences between the case- and control groups, we believe that our results are valid.
And caution about CFS diagnoses:
The overrepresentation of CFS among test-positives must be interpreted with care due to variability in how this diagnosis is made and the risk of confusing CFS with other conditions when filling in the questionnaire.
They also looked at sick leave rates, but unfortunately no durations:
Among the test-positives 12.0% reported taking any sick leave 4 weeks after test and until filling in the questionnaire 6-12 months later, compared to 7.7% of test-negatives (RD=4.32%, 95% CI 4.00-4.64%). Full-time sick leave was reported by 9.4% of test-positives and 6.5% of test-negatives (RD=3.20, 95% CI 2.88-3.47%), whereas part-time sick-leave was reported by 4.2% of test-positives compared to 1.7% of test-negatives (RD=2.43%, 95% CI 2.25-2.62%).
comment by Enceladus (willy-chertman) · 2022-01-23T18:12:57.054Z · LW(p) · GW(p)
General concerns which push me towards being much less cautious re: Long Covid than you, without getting into the specific details of studies:
- We have studied COVID far more than other diseases, so we may be finding stuff that either isn't real or more likely, occurs with other pathogens (we just hadn't bothered to look that closely before.)
- Upshot: worry less about Long Covid
- In general, a strong bias against preclinical/in-vitro work because I think that kind of lit is not very predictive of real-world issues.
- Upshot: worry less about Long Covid
- I'm more pessimistic than you about almost everyone getting Covid. Even with theoretical new vaccines for Omnicron or next-strain that approximate the original vaccine efficacy against the Wuhan strain, which was maybe 95% against severe outcomes and ~ 70-90% against infection in general, it seems difficult to achieve the herd immunity required for the more contagious strains. It is hard to find exact values but this article implies an R value of 4 or 5. That would require herd immunity threshold of 75-80%, which might be achieved with full next-gen vaccine uptake in the whole population, but that won't happen in the US because mandates are not going to happen on a large scale.
- But you could probably achieve herd immunity in a conscientious network of people, so perhaps this doesn't matter to you if you mostly socialize with those types of people.
- Upshot: avoiding COVID forever seems quite challenging
- Nobody who I know personally who had a mild (defined as not hospitalized) case of COVID (at least 30 people I know well) has had any long-term (more than 3 months) issues, and I have asked in detail. One person I know was in the ICU and does have long-term issues but that's expected for any ICU case from a respiratory disease. One person with a moderate case had a cough for 2 months after. From my limited interactions with LW/EA/rationalist types, I would guess my network is significantly less neurotic than what I'm guessing is your network and so they are less likely to experience psychosomatic symptoms .
- Upshot: worry less about Long Covid from personal experience
To balance that critique out, something that makes me think long-term issues from Covid are not so fanciful: a decent number of pathogens can cause weird long-term issues: EBV, measles, polio, Encephalitis lethargica, H. Pylori-->cancer. So COVID causing issues is not unprecedented.
Still, the idea of Covid causing accelerated aging in mild cases seems unlikely to me. I can't justify this intuition in-depth but my understanding is that when pathogens do cause long-term issues, it is relatively specific to a tissue or organ type, so I'm skeptical of broadly dysregulated issues from a mild infection.
Replies from: ChristianKl↑ comment by ChristianKl · 2022-01-23T20:55:57.281Z · LW(p) · GW(p)
To balance that critique out, something that makes me think long-term issues from Covid are not so fanciful: a decent number of pathogens can cause weird long-term issues: EBV, measles, polio, Encephalitis lethargica, H. Pylori-->cancer. So COVID causing issues is not unprecedented.
Quite crucially, we know that SARS did often cause long-term issues.
Still, the idea of Covid causing accelerated aging in mild cases seems unlikely to me. I can't justify this intuition in-depth but my understanding is that when pathogens do cause long-term issues, it is relatively specific to a tissue or organ type, so I'm skeptical of broadly dysregulated issues from a mild infection.
In the beginning of the pandemic there was a study that did heart scans that suggested that COVID infection generally cause lasting heart inflamation. It seems to me that there wasn't a lot of research to validate to what extend that's true and I see no reason to rule out that thesis.
Replies from: willy-chertman↑ comment by Enceladus (willy-chertman) · 2022-03-01T22:25:20.148Z · LW(p) · GW(p)
>>In the beginning of the pandemic there was a study that did heart scans that suggested that COVID infection generally cause lasting heart inflamation. It seems to me that there wasn't a lot of research to validate to what extend that's true and I see no reason to rule out that thesis.
My understanding is that similar findings occur in other diseases, especially in patients who are hospitalized, so I'm not sure that's novel to Covid.
Replies from: ChristianKl↑ comment by ChristianKl · 2022-03-02T19:29:36.843Z · LW(p) · GW(p)
Bad long term consequences aren't about whether there's something novel to COVID but whether COVID is similar to SARS which had very bad long term effects or whether it's not similar to SARS.
The studies that I remember saw such findings also in patients that were not hospitalized.
comment by Douglas_Knight · 2022-01-22T03:32:22.323Z · LW(p) · GW(p)
G. Overall deaths from everything have been very unusually high at points in 2021, even in 15-64 age group
Yes, all-cause mortality is up. We should look at all-cause mortality because it's what we care about, but when reasoning about causes, we should break it down by causes. Not all causes are up. The insurance executive says that young people are dying of random things months after covid. I'm happy to attribute unexplained deaths to the long-term effects of covid. But first you have to check that they don't have obvious explanations. The numbers I've seen is that it's mostly fentanyl. I'm pretty sure that's not covid. It might be lockdown, but I think it's just the continuing expansion of fentanyl (though that had flattened out for a couple years before the pandemic).
comment by MichaelStJules · 2022-01-17T00:19:01.041Z · LW(p) · GW(p)
Some other previous back of the envelope calculations (collected here [LW · GW]):
By AdamGleave [LW(p) · GW(p)] (2 shots and for Delta):
My new estimate from the calculation is 3.0 to 11.7 quality-adjusted days lost to long-term sequelae, with my all-things-considered mean at 45.
By Connor_Flexman [LW · GW]:
Replies from: MichaelStJulesThat being said, we can still roughly estimate risk from definitely having Delta. A healthy 30yo probably has about 4x (3x-10x) less risk than before, due to vaccination, despite Delta causing higher mortality. It almost entirely comes from Long COVID. In absolute terms this is ~4 expected days of life, plus 1/200th of your future productivity and vitality. You can shorthand this to about 1-4 weeks of life lost if you expect to otherwise live a full life—obviously, it costs less if you expect to live less less time. This translates to microCOVIDs at roughly 1 hour of your life lost every 1k-5k uCOVIDs. Risk of death goes up by 3x for every decade in age, but Long COVID probably only scales at ~~1.5x per decade, so for people over 60 mortality starts becoming more relevant. All these calculations are "creative" so please don't take them as definites.
↑ comment by MichaelStJules · 2022-01-17T23:03:28.746Z · LW(p) · GW(p)
Also, by Elizabath (I think her LW post [LW · GW] was not updated since some corrections were made).
I would focus on the UK metareview she looked at, since it should better capture the risk of severe brain fog and fatigue. The intelligence study estimated the average drop in IQ by acute symptom severity, but I think there are decreasing marginal returns to IQ, so I'm more worried about a small risk of a big drop (or being unable to even focus on doing an intelligence test, due to brain fog or fatigue), and Taquet et al focused on neuro and psych diagnoses that did not include brain fog or fatigue. Here's what she had to say based on the metareview:
A UK metareview found the prevalence at 12 weeks of symptoms affecting daily life ranged from 1.2% (average age: 20, minimum 18) to 4.8% (average age: 63). The cohort with average age 31 had a mean prevalence of 2.8%., which is is well within the Lizardman Constant. This is based on self-reports on survey data, which will again exclude asymptomatic cases, so even if you treat it as real, you need to discount it down to 2.8%.
On the other hand, medicine is notoriously bad at measuring persistent, low-level, amorphous-yet-real effects. The Lizardman Constant doesn’t mean prevalences below 4% don’t exist, it means they’re impossible to measure using naive tools.
I think this gives us a fairly reliable upper bound on the risk of severe long COVID cases ("affecting daily life", or in the study's wording, "limiting day-to-day function") for healthy people in the given age groups, and a more reliable upper bound than Matt Bell's, since
- Matt Bell's started from overall prevalence estimates that don't depend on severity and then made adjustments for severity based on other studies, and this seems more prone to bias/error, and
- the above study is more directly attempting to measure what we care about, and seems unlikely to be biased downwards.
There's no comparison group here in this metareview, and this is an absolute risk estimate based on self-reported symptom duration, according to NICE's definition of post-COVID-19 syndrome (PCS), which is supposed to rule out alternative diagnoses at least, but that can still leave room for people misreporting or not knowing that there is an alternative explanation:
Post-covid-19 syndrome—Signs and symptoms that develop during or after an infection consistent with covid-19, present for more than 12 weeks and are not attributable to alternative diagnoses.
This is also pre-vaccine, and pre-Delta (and so, of course, pre-Omicron). It's also not clear exactly how severe "limiting day-to-day function" is supposed to be, without looking further into it.
comment by faul_sname · 2022-01-21T20:31:05.991Z · LW(p) · GW(p)
According to a massive controlled study published in Nature (more readable summary here). It also looks like they are saying that this is for non-hospitalized covid patients, though the paper is confusing to me.
I am also a bit confused by what this study is trying to show. In Figure 3 it shows that a lot of things occur more frequently in patients who tested positive for COVID than in their matched controls, more in those hospitalized than that, and yet more in those admitted to the ICU. Per their methods section, this was measured by comparing the number of patients first reporting that condition within the 6 month period following a COVID-19 diagnosis vs the 6 months following (not sure) for everyone else in the VA system.
Looking at their data, they observe that people with a positive COVID-19 test are 1.17x, 2.34x, and 3.44x more likely for non-hospitalized, hospitalized non-ICU, and ICU-admitted patients respectively, to report obesity in the 6 month period than the COVID-19 negative controls. They cite this as an excess burden of obesity of 3.37, 26.15, 46.9 people per thousand among those three groups, which gives a baseline risk of about 1.95% for the control group reporting obesity within their 6 month period, if I'm doing my math right.
So taken at face value, the average person in the VA system has about a 2% per 6 months chance of becoming obese, while the average person admitted to the ICU has about a 7% chance of becoming obese in the next 6 months. I can come up with two possible explanations for that:
- People who are admitted to the ICU gain about 3.37x more weight, on average, than people who do not get COVID-19, and as such are about 3.37x more likely to become obese.
- Getting COVID-19 has very little effect on your weight, but within the group of people who are not obese, the people who are closer to the threshold of obesity are more likely to be admitted to the ICU for COVID-19.
I don't have hard evidence one way or the other, but I did some searching for evidence that COVID-19 causes weight gain, and while I found a large number of articles talking about how people are gaining weight under lockdown, I didn't find any discussing weight gain from COVID-19 directly. Additionally, my prior is that controlling for confounding factors is really really hard, and so even for a study published in Nature I would not be surprised if the authors failed to perfectly control for those confounding factors.
I'd be interested to see what you get if you
- Look at weight changes in a group of people who tested positive vs negative for COVID-19 in a specific narrow period, to see if the COVID-positive people experienced more weight gain over that period, controlling for weight at the start of that period (and if so, whether that weight gain was correlated with disease severity).
- Reproduce this study, except look the relative risk of experiencing one of these negative sequelae in the 6 month period before a positive COVID-19 diagnosis (if this method successfully controls for confounding factors, doing this should show a hazard ratio very close to 1 for all conditions, assuming that getting COVID can't cause you to experience negative health outcomes in the past).
comment by ChristianKl · 2022-01-18T12:53:47.475Z · LW(p) · GW(p)
I remember from early in the pandemic studies suggesting that there's measurable long-term heart inflammation in many cases. That seems to be one plausible mechanism for long-COVID that's less subjective. Does anyone read the literature to have a more recent idea of this?
comment by bortrand · 2022-01-18T07:48:29.439Z · LW(p) · GW(p)
This is very interesting. I find this somewhat persuasive and am updating in the direction of being more afraid of getting covid. That being said, I think I'm still pretty far from your level of concern. I can think of three places where I think we may disagree.
- I find your example in K very odd, in that it requires 100/900 people without covid to get illnesses that are as bad as long covid, but only 10/100 people who had covid to have similarly bad symptoms from long covid. It would be weird if we lived in a world where people without covid are so much more likely to get other illnesses that they're more likely to have symptoms that could be confused for long covid then people who actually had covid (if this was the case for some reason, that would also make covid way less scary), and I think your assumption breaks down if the scenario was set up differently.
- Judging by the effect size of vaccines on hospitalizations and deaths, my priors would be that they would be more than 50% effective against long covid (or at least the really bad long covid that seems most worrisome). The study in C makes me update a little towards 50% but not that much. One potential issue is that e.g. if 25% of the unvaccinated long covid were psychosomatic, and vaccination does not affect the probability of psychosomatic long covid, then an observed reduction of 50% from vaccination, would mean a 67% reduction of non-psychosomatic covid. I would guess Omicron is also less scary, given that it seems like it doesn't infect the lungs nearly as much, but I'm less confident on that.
- This is somewhat specific to me, but I suspect a lot of the people reading this also fit into the group of <40 yo, healthy, and not obese, so maybe it applies to others as well. Given how big the differences are between demographics for covid, I find anything that looks at the population-level to be potentially misleading for me. One thing that makes me feel less worried is looking at the results for professional athletes. There's an obvious selection bias, there, but I think it's better than having a non-obvious selection bias in basically any other study, and I suspect my risk factors are more similar to professional athletes than to the average American (given that risk scales superlinearly with age, weight, and medical history, it's probably the case that a median American is closer to a professional athlete than to the mean American, and I'm younger and probably healthier than median). The other nice thing about professional athletes is that their health is tracked very closely (though unfortunately, I don't see much work being done to compile and study it altogether). I feel like this is similar to the "How many people do I actually know that have been affected by this?" approach. From what I can tell, >50% of athletes in the four major US sports seems to have had covid already, and I can only find a few cases of long covid per sport. That seems approximately consistent with long covid risk being between 0.1%-1%, which isn't far off from some of the estimates being quoted. Notably, though, I'm having trouble finding any cases that have come from after vaccinations were widely available. There could be all sorts of confounders here, the most obvious being that no one would yet be talking about a long covid cases from an Omicron infection they got a few weeks ago, but the fact that these leagues are not being devastated by long covid, despite having professionals who are very dependent on their lung function and energy levels makes me feel reasonably good about my own prognosis.
That being said this report that you referenced suggests the odds ratios between demographics are not as extreme for long covid as they are for hospitalizations or deaths, which would mean maybe I'm not that much safer than an average person. That could potentially also be explained by a fairly uniform distribution of psychosomatic cases, though.
comment by Gunnar_Zarncke · 2022-01-17T08:28:13.271Z · LW(p) · GW(p)
The key point for me is the Value of Information of waiting some more. Many people will get Omicron soon and we will have more data.
comment by Lukas Finnveden (Lanrian) · 2022-01-17T06:12:49.363Z · LW(p) · GW(p)
A French study found that long covid is barely associated with having had covid according to an antibody test, yet associated with believing one has had covid (which itself is unrelated to the antibody test results).
Sorry, are you claiming that "belief in covid" is uncorrelated with antibody test results? I think:
- That's a wild claim (people are seriously no better than random at determining if they've had covid?).
- As far as I can tell, the study doesn't claim that.
- At a glance, the most important result of the study seems to be that antibodies are correlated with long covid as long as you don't control for belief-in-covid; but antibodies are not associated with long covid once you do control for belief-in-covid. That makes a lot of sense if antibodies and belief-in-covid is very correlated with each other, but is harder to explain otherwise.
Relatedly, your story for why the french study doesn't imply that covid is psychosomatic is way more extreme than it needs to be. Claiming that you have long covid is totally associated with having covid, as long as you don't control for belief-in-covid. See e.g. this post [LW · GW].
Edit: See also the comment I wrote here [LW(p) · GW(p)].
Replies from: Daniel V↑ comment by Daniel V · 2022-01-17T16:00:09.770Z · LW(p) · GW(p)
Right, there is a ton of misunderstanding regression floating around on this issue it seems. Yet, one would still think that Having covid would be more predictive of Long covid than Believing you've had covid, since Believing and Long ought to be correlated only through their shared association with Having (common cause rather than mediation). The fact that this is not the case could indicate that people with chronic conditions come to think they Had covid (discussed at the end of the study) or that the measure of Having covid is not that good (see Siebe's comment), or that it's psychosomatic (loose usage of the term), or something(s) else.
Adding to the uncertainty is that "less than half of those with a positive serology test reported having experienced the disease." This is especially troublesome since participants were informed of their serology results prior to the self-reports, so that's some weird denial (or misunderstanding). However, that doesn't mean they are unassociated! They are associated! (Table 2) Only 2% of seronegatives believed they had covid, but 42% of seropositives did. Having-->Believing, so that's good at least.
↑ comment by Lukas Finnveden (Lanrian) · 2022-01-17T16:14:30.137Z · LW(p) · GW(p)
Yet, one would still think that Having covid would be more predictive of Long covid than Believing you've had covid, since Believing and Long ought to be correlated only through their shared association with Having (common cause rather than mediation). The fact that this is not the case could indicate that people with chronic conditions come to think they Had covid (discussed at the end of the study) or that the measure of Having covid is not that good (see Siebe's comment), or that it's psychosomatic (loose usage of the term), or something(s) else.
Or that long covid is mainly caused by symptomatic covid, and Believing is a better predictor of symptomatic covid than antibody tests. Which seems pretty likely.
Replies from: Daniel Vcomment by Florin (florin-clapa) · 2022-01-16T21:27:56.377Z · LW(p) · GW(p)
G. Overall deaths from everything have been very unusually high at points in 2021, even in 15-64 age group
This is wrong. Excess death increased significantly compared to the baseline only in the 45+ age groups. OWID mislead you by lumping in a bunch of age groups together.
https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm (select "Weekly Number of Deaths by Age")
https://www.euromomo.eu/graphs-and-maps
If everyone believed that covid was bad enough to get, it would die out in a month (possibly with terrible economic downsides for a month).
The same thing could be achieved without the economic downsides if everyone wore respirators [LW · GW].
Replies from: benwr↑ comment by benwr · 2022-01-16T22:17:16.242Z · LW(p) · GW(p)
Hm. On doing exactly as you suggest, I feel confused; it looks to me like the 25-44 cohort has really substantially more deaths than in recent years: https://www.dropbox.com/s/hcipg7yiuiai8m2/Screen Shot 2022-01-16 at 2.12.44 PM.png?dl=0 I don't know what your threshold for "significance" is, but 103 / 104 weeks spent above the preceding 208 weeks definitely meets my bar.
Am I missing something here?
Replies from: florin-clapa, florin-clapa, JesperO↑ comment by Florin (florin-clapa) · 2022-01-17T06:37:23.538Z · LW(p) · GW(p)
The infection fatality rate might be an even better way to quantify the risk of death. The IFR for covid in the 15-64 age groups before September 2020 was 0.75% at the higher end of the range. Older age groups had IFRs ranging from 2.5% to 28%. The IFR of the flu doesn't usually go over 0.1%, although this is an average and the accuracy of the stat itself is questionable (from other sources I've seen).
↑ comment by Florin (florin-clapa) · 2022-01-17T04:20:51.137Z · LW(p) · GW(p)
Although it might not be entirely insignificant, it seems a lot less significant than it would appear. Eyeballing it, there seems to be about 100k excess deaths in the 25-44 age group (usually, it's about 300k total deaths for 104 weeks) out of a total of 950k excess deaths. That's a 25% increase of excess deaths compared to the baseline, but nowhere the near 40 to over 60% peaks that an uncritical reading of OWID's chart would suggest. Also, the 25-44 group is about 26% of the US population, yet has suffered only 10% of the deaths, whereas the 45+ groups (harder to eyeball just the 45-64 group) are 41% of the pop and have suffered from 90% of the deaths. And since covid mortality increases the older one gets, a person in their late 20s would likely have less chance of dying than a person in their early 40s.
This is perhaps clearer in terms of risk of death due to covid by age group (compared to 18-29 year olds):
30-39: 4x
40-49: 10x
50-64: 25x
65-74: 65x
75-84: 150x
85+: 370x
↑ comment by Daniel V · 2022-01-17T16:23:29.699Z · LW(p) · GW(p)
Florin's right that the 15-64 age group doesn't pain a clean picture of the actual numbers since it combines very different excess death rates, but even the 25-44 group experienced a serious increase. Rather than Katja being "wrong," they are very much right.
"For the next 2 years, you will have a 25% higher risk of death than usual" is not a high absolute risk of death, but that shift from baseline is not just "not entirely insignificant" either.
↑ comment by Florin (florin-clapa) · 2022-01-17T21:46:53.051Z · LW(p) · GW(p)
I think we mostly agree, although I still think using the OWID chart is wrong or at least very misleading.
While the 25% is okay in aggregate, there does seem to be a 60% peak in mortality in 2021 at week 35 for the 25-44 group. So, I was wrong about that. However, the 45-64 group has only a 37% peak in mortality in 2021 at week 36, and using the raw data, I calculated (just averaged and didn't do any fancy weighting) that there was only a 18% increase in excess death overall.
But that's not the end of the story.
2020-2021, 25-44: 757,645 (single year average)
2015-2019, 25-44: 542,284 (single year average)
Difference: 215,361 (2x what eyeballing the chart suggests, but whatever), 28% increase in excess deaths
2020-2021, 45-64: 2,632,764 (single year average)
2015-2019, 45-64: 2,162,344 (single year average)
Difference: 470,420, 18% increase in excess deaths
Each age group makes up about 26% of the US population, but the 45-64 group has more than double the risk of death, even though it has a lower increase (relative to pre-2020 years) in excess deaths. So, the focus on the relative (what the OWID chart is about) rather than the absolute increase in death is misleading.
The IFR data (mentioned in another comment) also seems to suggest this.
↑ comment by JesperO · 2022-01-17T06:53:04.554Z · LW(p) · GW(p)
Aren't those excess deaths just the direct covid deaths, from the unlucky few younger people who got covid and died from it?
Replies from: florin-clapa↑ comment by Florin (florin-clapa) · 2022-01-17T19:13:28.752Z · LW(p) · GW(p)
Excess deaths are deaths from all causes. But it's usually assumed that they're mostly covid deaths.
Replies from: pktechgirl↑ comment by Elizabeth (pktechgirl) · 2022-01-17T19:24:58.190Z · LW(p) · GW(p)
I think that assumption is inaccurate, and is becoming more inaccurate over time. Lockdown is also hard on people and contributes to the excess deaths.
Replies from: arunto, florin-clapa↑ comment by Florin (florin-clapa) · 2022-01-17T22:41:03.686Z · LW(p) · GW(p)
CDC data seems to suggest that 269,014 excess deaths (select "Total number above average by cause") aren't due to covid out of a total of 952,707 total excess deaths (select "Number of Excess Deaths"). That means 72% (most) might be covid-caused.
Replies from: pktechgirl↑ comment by Elizabeth (pktechgirl) · 2022-01-17T23:18:31.579Z · LW(p) · GW(p)
It looks like those deaths are "with covid" not necessarily "due to covid". I think that was a reasonable approximation at first, but it makes it a bad tool for tracking when covid becomes less dangerous and more widespread.
However the fact that excess deaths are spiking with covid prevalence is pretty suggestive.
comment by arunto · 2022-01-16T12:30:13.940Z · LW(p) · GW(p)
In general, I agree with your view that one should try not to get Covid (Unless the individual costs for trying not to get it are very high, which would depend on the individual life circumstances. Since here in Germany many things are closed down anyway, for me the costs are smaller than the benefit of playing ist safe). Having said that, short remarks about two of your points:
G. Here it is interesting to look at different countries. For me the default in the tool was UK and Germany, and the differences in excess mortality for the age group 15-64 were huge. I am not sure whether that can only be explained by different Covid rates in different countries.
Q. On a short time-scale one important factor could be how long ago you were boostered (assuming you have got 3 vaccinations). With a booster very recently (maybe a couple of weeks) it could be better to be infected now than in 3 months. (I still think it would be even better not be infected now or in 3 months, but depending on the individual costs of not getting infected the timing of the booster could be a relevant factor for some people).
comment by William_S · 2022-01-18T19:09:48.186Z · LW(p) · GW(p)
Is there any work going on that seems at all likely to decrease risk of getting long covid conditional on getting infected, beyond current vaccines? E.g. alternative vaccines with a story to suggest why they might decrease risk, evidence of Paxlovid or other treatments decreasing risk, other targeted research programs
.png?width=960&height=720&fit=bounds)
.png?width=960&height=720&fit=bounds)